A centralized trophoblastic disease program was launched at Mount Sinai Hospital in July 2018 to care for women with molar pregnancy, abnormal b-hcg levels not related to pregnancy and gestational trophoblastic neoplasia. The program is led by Dr. Bouchard-Fortier who has developed an expertise in management of trophoblastic disease. Read more about the trophoblastic disease program. To refer a patient, click here.
Endometrial cancer (cancer of the uterine lining) is the most common gynecologic malignancy in developed countries and has been rising over the last 15 years. Definitive treatment and standard of care for endometrial cancer is surgical removal of uterus, tubes, and ovaries. About five per cent of cases occur in women under the age of 40 and results in fertility challenges for women who still want to preserve fertility. However, for highly select group of young patients with low grade disease confined to the endometrium alternative treatment with hormonal methods such as progesterone or levonorgestrel-releasing intrauterine system (IUD) may be a reasonable temporary option to provide a window of opportunity to achieve pregnancy.
Fertility conserving treatment is only suitable for select group of patients and we follow these patients closely in collaboration with Reproductive Endocrinology & Infertility specialists to concurrently manage other treatable risk factors and to optimize the probability of a successful pregnancy.
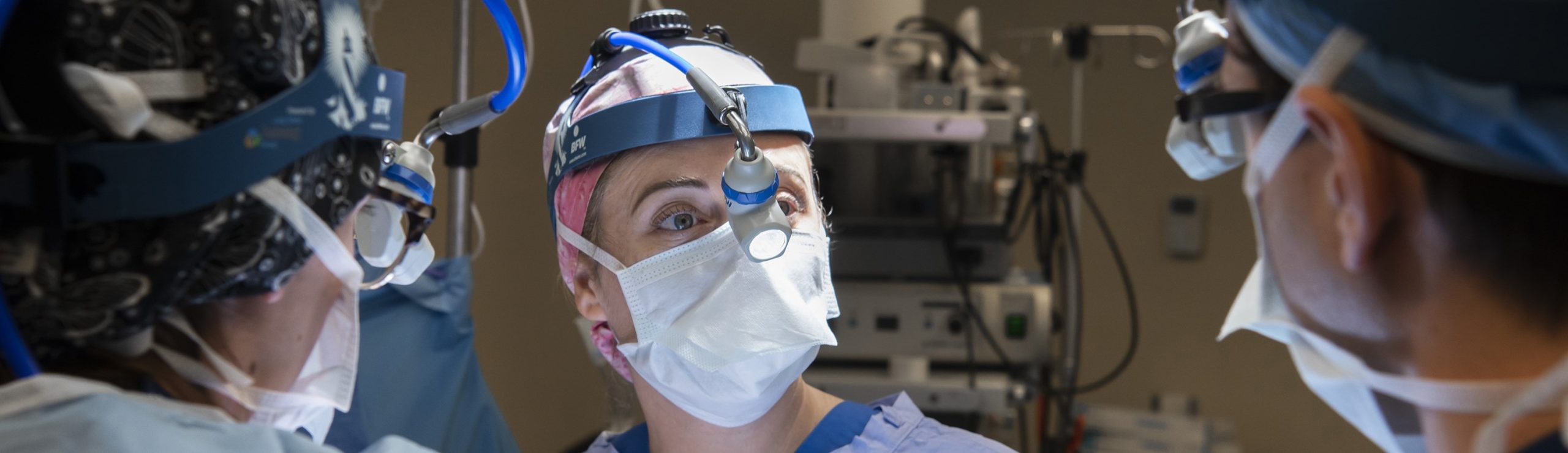
Robotic surgery, or robot-assisted surgery, is a type of minimally-invasive surgery that allows doctors to perform many types of complex procedures through several small incisions (cuts) on the skin. This technology allows the greatest precision and control compared to conventional laparoscopic techniques.
The robotic surgical system includes a camera arm and mechanical arms with surgical instruments attached to them. The arms are controlled by the surgeon, who is seated at a computer console near the operating table. The console provides the surgeon a with a high-definition, magnified, 3-D view of the abdominal cavity. There are many benefits to robotic surgery, including reduced recovery time and shorter hospital stay.
Toronto General Hospital is one of the few hospitals in Toronto equipped with a robotic surgical platform. At UHN, we have four surgeons who each have completed hundreds of complex robotic cases and are experts in the field of robotic surgery.
Click here to watch a video about minimally-invasive hysterectomy.
In the general population, there is 1.5% life-time risk of developing ovarian cancer. Despite extensive research in this field, ovarian cancer remains the most lethal gynecological malignancy. There is no effective screening test and no symptoms of early stage disease. Multiple studies have shown that for the well selected group of patients, aggressive surgical management followed by chemotherapy and/ or maintenance treatment can improve survival.
At UHN, we are maximizing efforts to help these patients. As of October, 2018, we initiated the “comprehensive ovarian cancer program”. Every referral with suspected or diagnosed advanced ovarian cancer is prioritized and booked into clinic within 7 business days. We have a program navigator who contacts the patients prior to their clinic appointment to assure imaging are already done or booked urgently. We arrange for a biopsy to be carried out in a short term interval, to minimize any delays to diagnosis/ treatment. At the time of the clinic appointment, the patient and family meet with the gynecologic oncologist as well as with our nursing team and the program navigator. The patients are being offered to participate in clinical trials if they are interested and eligible.
Each case is then presented in our Ovarian Cancer Multi-disciplinary Cancer Conference, which includes surgeons, expert radiologists, medical oncologists and the program navigator. We carefully discuss each case based on multiple criteria to decide about next steps.We aim to deliver the best treatment in the most effective, prompt and compassionate way. We have a leading surgical team, front line systemic treatment options and well-trained support team to assure no questions are left unanswered.
Since the implementation of the Ovarian Cancer Surgical Program, our team has worked hard to achieve an efficient timeline through the program by lowering wait times for initial consult and start of treatment. Once referred to our program, patients are prioritized and booked for primary clinic consultation within 7 business days. Additionally, the average time to begin treatment has also decreased. In order to continue achieving our goal to deliver the best treatment in the most effective, prompt and compassionate way, we continually ask our patients for their feedback regarding their experience through our program. To date, our patients have expressed great appreciation towards our clear communication and continuous efforts in preparing them for their journey ahead. Patients provided the following feedback when asked about their experience with our Ovarian Cancer Surgical Program:
Read more about ovarian cancer from Dr. Taymaa May.

The Familial Ovarian Cancer Clinic (FOCC) and FOCC-Aftercare clinics at Women’s College Hospital provide expert and evidence based clinical care for women at elevated risk for hereditary ovarian and fallopian tube cancers. Clinical care includes the full spectrum of gynecologic care specific to our population: patient centered contraception counselling, liaison with fertility specialists, counselling on ovarian cancer risk reduction, risk reduction surgery, and menopausal aftercare. Patients seen in the FOCC clinic will be followed until the first post-operative appointment.In collaboration with the Department of Gynecologic Oncology at Princess Margaret Hospital, the Women’s College Research Institute, and the WCH High Risk Breast Clinic, the clinic utilizes an interdisciplinary model of care to provide counseling, risk reducing surgery, and comprehensive menopause management to women who are at risk for ovarian or fallopian tube cancer. The program is directed by Dr. Marcus Bernardini and Dr. Michelle Jacobson. Learn more about the FOCC.
Gynecologic cancers are particularly devastating when diagnosed in young women and children and we have a devoted team dedicated to caring for these patients. When young people undergo life-saving cancer therapies, they are at risk of infertility and its long-term effects. We have developed expertise in management of rare gynecologic malignancies presenting in young women and children with a focus on fertility preserving minimally invasive surgery. Realizing that there are distinct differences in care for these populations, we collaborate with the pediatric team at the Hospital for Sick Children to develop unique, multidisciplinary management protocols for these unique patients.
 For women with cervical cancer, treatment used to involve the complete removal of the cervix and uterus, leaving them cancer-free but without the ability to have children, says Dr. Taymaa May. But increasingly, surgeons like Dr. May are using a revolutionary technique called a radical trachelectomy to treat cervical cancer, leaving the cervix, the upper part of the vagina and supporting tissues intact. The six-hour, computer-assisted surgery, using the Da Vinci robot, allows for minimally invasive laparoscopic incisions, as well as tissue and lymph node removal. “The patients have smaller incisions in their abdomen, less pain and they can go home the same day,” says Dr. May. In the past they would have been hospitalized for four or five days.
For women with cervical cancer, treatment used to involve the complete removal of the cervix and uterus, leaving them cancer-free but without the ability to have children, says Dr. Taymaa May. But increasingly, surgeons like Dr. May are using a revolutionary technique called a radical trachelectomy to treat cervical cancer, leaving the cervix, the upper part of the vagina and supporting tissues intact. The six-hour, computer-assisted surgery, using the Da Vinci robot, allows for minimally invasive laparoscopic incisions, as well as tissue and lymph node removal. “The patients have smaller incisions in their abdomen, less pain and they can go home the same day,” says Dr. May. In the past they would have been hospitalized for four or five days.
But the biggest advantage of radical trachelectomy is that it preserves fertility. “(Women) have the option of carrying a pregnancy at a later time,” explains May, who’s one of fewer than 10 surgeons in Canada to have performed this surgery. She has also expanded the procedure to treat another rare cancer that affects women and girls under age 18: rhabdomyosarcoma of the cervix, an aggressive cancer that forms in muscle tissue.
Care
Providing multi-disciplinary expert care of patients and their families during treatment for a gynecologic malignancy.
Research
Dedicated to advancing the field through scientific collaboration and research innovation.
Education
Committed to expanding gynecologic cancer awareness and developing skills and knowledge of medical trainees.
Website created by Blue Ocean Marketing Inc, Digital Advertising Agency Toronto.
Gynecologic Oncology Surgery Team